Liver diseases and liver transplants
Hepatitis, liver failure, liver cancer, alcoholic liver diseases
At a Glance:
What is the liver? What are its functions?
What are the types of liver diseases?
What are the causes of liver disease?
Who is more prone to develop liver disorders? What are the risk factors for liver diseases?
What are the stages of liver diseases?
What are the complications of liver disorders?
What are the signs and symptoms of liver disorders?
When to seek medical consult for liver disease?
How are liver diseases diagnosed?
What is the liver? What are its functions?
Liver is one of the vital organs of the body that sits on the right side of the stomach. It is reddish-brown, rubbery organ that is well protected beneath the rib cage. The liver is the largest internal organ in the body and is responsible for many critical functions within the body. Damaged or diseased liver results in the loss of those functions and significant damage to the body. Usually, more than 75% or three quarters of liver tissue needs to be affected before a decrease in function occurs.
The two large sections of the liver, called as right and left lobe, along with pancreas and gallbladder help to digest, absorb and process food. Liver secretes bile which is essential for digestion and makes protein which is essential for clotting and other functions. The blood coming from the digestive tract reaches liver for removing toxins and metabolizing drugs before it is supplied to the body.
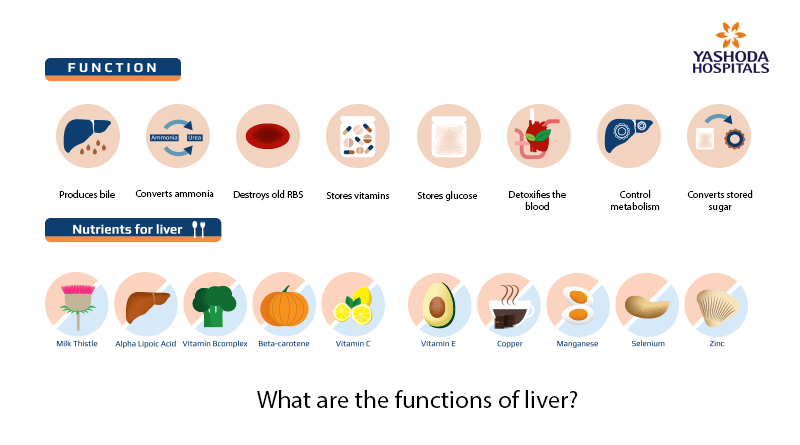
Some of the common functions of the liver are:
- Produces bile a substance needed to digest fats
- Converts ammonia to urea which is vital in metabolism
- Destroys old RBC
- Stores Vitamins and iron
- Stores and releases glucose
- Controls metabolism
What are liver diseases?
Liver disease or hepatic disease is any condition that damages the liver and poorly affects its functioning. Longstanding or untreated liver disease can cause serious, irreversible damage to the liver.
Liver damage may be caused in several ways:
- Inflammation of liver as seen in hepatitis
- Obstruction to bile flow as seen in cholestasis
- Deposition of excess cholesterol as seen in steatosis
- Deposition of excess fat as seen in fatty liver and liver enlargement
- Scarring and damage to liver tissue as seen in fibrosis and cirrhosis
- Cancerous cells infiltrating as seen in hepatocellular carcinoma
What are the types of liver diseases?
According to NHS, there are over 100 types of liver diseases. Some of the common types of liver diseases are –
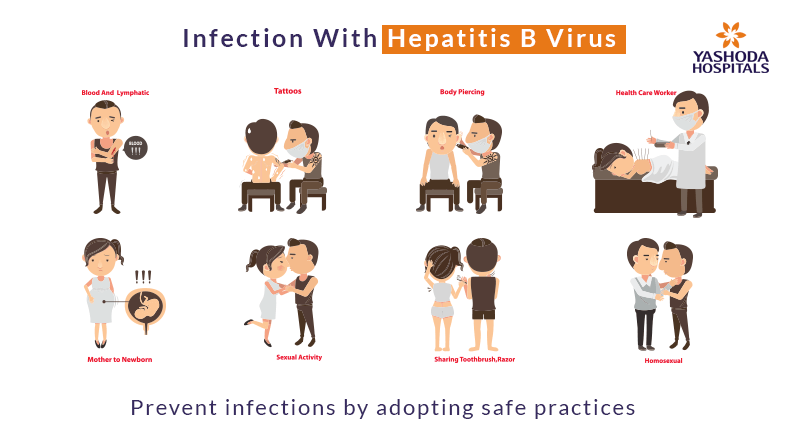
- Viral (Infectious) hepatitis: Hepatitis literally means inflammation (swelling and reddening) of the liver. It is caused by the hepatitis viruses, Hepatitis A, B, C, D and E. Hepatitis A and B are preventable by vaccines.
- – Hepatitis A is often mild and patients usually make a full recovery in 2 months without intervention. There are safe and effective vaccinations against Hepatitis A virus (HAV).
- – Hepatitis B: The liver damage may progress from inflammation to cirrhosis and hepatocellular carcinoma. There is no cure for HBV. However, protective vaccines are available
- – Hepatitis C: Similar to HBV, hepatitis C can cause severe liver damage, cirrhosis and lead to hepatocellular carcinoma (a form of liver cancer).
- Liver cysts: Liver cysts are fluid-filled spaces in the liver. They are usually symptomless and do not need treatment. Larger cysts may cause pain and discomfort which require drainage and removal of the cysts.
- Liver Cancer: Liver cancer is the growth and spread of abnormal, unhealthy cells in the liver. Hepatocellular carcinoma is the most common type of liver cancer. Cirrhosis and Hepatitis B are the leading risk factors for liver cancer.
- Hereditary diseases: Some of the genetic liver diseases include,
- – Wilson disease is the condition of excess copper accumulation in vital organs.
- – Hemochromatosis is the condition of excess iron retention in the body.
- Cirrhosis: Cirrhosis is the scarring of the liver where the soft healthy tissues are replaced with hard scar tissue. Cirrhosis may result from longstanding inflammation from infections, heart disease, or continuous injury.
- Fatty liver, there is excess fat stored in the liver. It can either be an alcohol-related fatty liver disease (ALD) or Nonalcoholic Fatty Liver Disease (NAFLD).
- – Alcohol-related (fatty) liver disease is marked by alcoholic hepatitis and alcoholic cirrhosis.
- – Non-alcoholic fatty liver disease (NAFLD) is either simple fatty liver or Non-Alcoholic SteatoHepatitis (NASH). In simple fatty liver, the liver cells are inflamed. However, in NASH, the liver cells are further damaged with fibrosis, cirrhosis and even cancer of the liver.
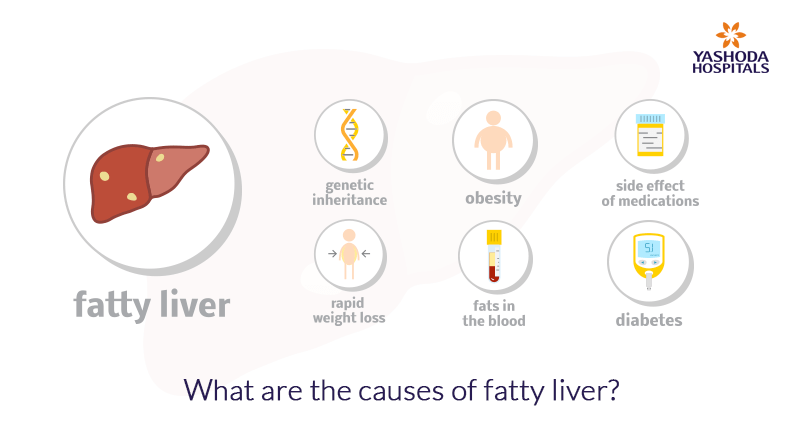
What are the causes of liver disease?
Commonly associated causes of liver diseases include:
- Infection – Hepatitis virus
- Problems in the immune system – autoimmune hepatitis, primary biliary cirrhosis
- Genetics
- Cancer and other growths
- Chronic alcohol abuse
- Drug induced liver damage
- Fat accumulation in the liver
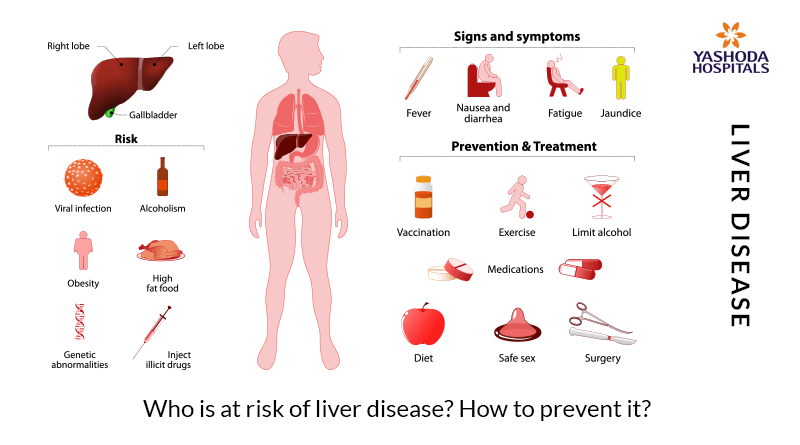
Who is more prone to develop liver disorders? What are the risk factors for liver diseases?
People with the following risk factors are more prone to develop diseases:
- Excess alcohol intake
- Shared needles for injections (common in drug abusers)
- Body piercing and tattooing with unsterilized needles
- Exposure to an infected person’s blood and body fluids
- Unprotected sex
- Exposure to harmful chemicals or toxins
- Underlying medical conditions like diabetes, obesity etc.
What are the stages of liver diseases?
There are several conditions that are diagnosed with liver disease. However, the damage to the liver follows a consistent pattern from the initial stages to advanced stages of the disease.
Stage 1 – Inflammation: Irrespective of the cause of the liver disease, the liver and the liver ducts get inflamed (swollen, reddened) causing abdominal pain. If left untreated, inflammation can cause further damage to the tissues. Inflammation of liver is often treated completely.
Stage 2 – Fibrosis: In many cases, liver diseases may not be diagnosed until stage 2. Fibrosis of liver is marked by scarring in the tissues which may affect blood flow to liver and liver functions. With treatment, the scarring is healed and further damage is prevented.
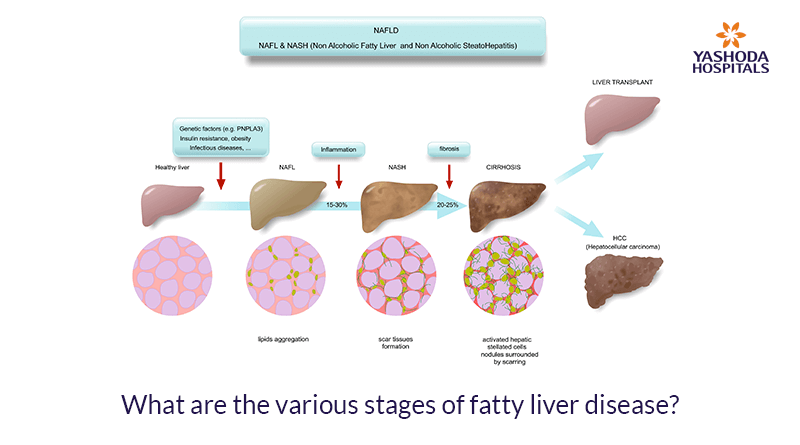
Stage 3 – Cirrhosis: Cirrhosis of the liver is a chronic (longstanding) condition marked by permanent scarring that obstructs blood flow to the liver. The most common causes of cirrhosis in the US are chronic hepatitis C infection and alcoholic liver disease. This stage of liver disease is serious and the treatment must begin immediately to halt the progress of the liver disease and the damage. Liver cirrhosis causes decompensation of the liver and can cause serious symptoms and comorbid conditions which need to be managed with prompt care. It is important to protect the healthy tissues that are left to retain the liver functions intact.
Some of the alarming changes in the decompensated cirrhosis (liver disease) include portal hypertension, esophageal varices (dilated, ballooned veins), ascites (accumulation of fluid in the abdominal cavity) and gastrointestinal bleeding. The patient may experience extreme fatigue, confusion, personality changes, extreme sleepiness, reduced urination (an indication of kidney failure), high fever (an indication of possible abdominal infection), swelling in the extremities, wasting of muscles in the extremities, hand tremors, shortness of breath, pale/yellow skin, weight loss, loss of appetite.
Stage 4 – Liver failure: Liver failure, also known as liver insufficiency, is the condition wherein the normal functions of the liver begin to fail. Large part of the liver is affected by irreparable damage and thus the liver fails to perform the routine activities. Based on the causative factors, liver failure may either be acute (rapid development usually in patients without known prior liver disease), chronic (slow progress due to long-term, excessive alcohol intake, hepatitis B, C etc.), or acute-on-chronic liver failure (ACLF).
- Acute liver failure can be life-threatening and needs immediate medical attention. Usually, it develops within a few days due to over dosage or poisoning from medications such as paracetamol, infections (hepatitis B or C), acute fatty liver of pregnancy, etc.
- Chronic liver failure develops slowly over many years due to long-term exposure to excessive alcohol, infections.
- Acute-on-chronic liver failure occurs as a result of alcohol misuse or infection.Patients with ACLF can be critically ill and require intensive care and sometimes liver transplants.
- End-stage liver disease (ESLD): Extensive damage most commonly as a result of cirrhosis or long-term infections results in chronic liver failure. Patients with ESLD show symptoms and complications that affect survival and quality of life.
What are the complications of liver disorders?
The complications and outcomes of liver disease depend on the underlying cause. However, a long-standing and untreated liver disease can develop into a life threatening liver failure.
Some of the complications of liver disorders include:
- Swelling (edema) and accumulation of fluids in the abdomen (ascites)
- Bruising and bleeding in liver
- Portal hypertension (high pressure in portal veins which supply to liver from GI tract, pancreas, gallbladder and spleen)
- Enlarged spleen (splenomegaly)
- Jaundice
- Hepatic encephalopathy
- Insulin resistance and type 2 diabetes
- Liver cancer (hepatocellular carcinoma)
Worsening immunity (Immune system dysfunction) and increased risk for infections.
What are the signs and symptoms of liver disorders?
Most types of liver diseases do not show any signs and symptoms in the early stages. The symptoms are visible when the liver is already damaged or scarred. Some of the common signs and symptoms of liver disorders are:
- Chronic tiredness
- Decreased appetite (hunger)
- Discoloration of the urine
- Easy bruising
- Leg and ankle swelling
- Nausea or vomiting
- Itchy skin
- Swelling and pain in the abdomen
- Tar coloured or clay-like pale stools
- Yellowish coloration of eyes and skin; known as jaundice
When to seek medical consult for liver disease?
In the initial stages, liver disease may not show any symptoms to seek medical care. However, see a gastroenterologist if you are prone to develop liver disease and you have symptoms of cirrhosis, such as:
- Feeling very tired and weak all the time
- Loss of appetite – which may lead to weight loss
- Loss of sex drive (libido)
- Yellow skin and whites of the eyes (jaundice)
- Blood vomiting
- Black colored stools
How are liver diseases diagnosed?
It is important to determine the underlying cause of liver disease. Your physician or gastroenterologist shall determine the diagnosis on the basis of:
- Medical and personal history
- Physical examination
- Blood tests
- – Liver function tests
- – Complete blood count (CBC); blood clotting tests; lipase; electrolytes and creatinine, etc.
- Imaging studies (CT scan, MRI and ultrasound)
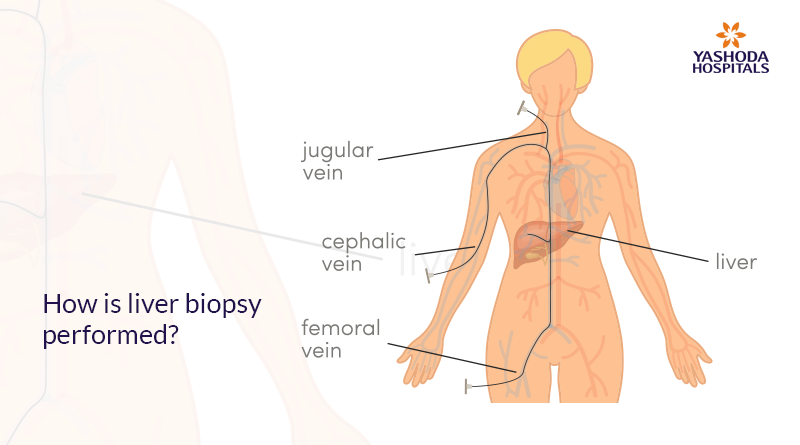
- Liver biopsy
What is the treatment for liver disorders?
Treatment of liver diseases depends on the underlying cause of liver damage. Treatment course also depends on the stage and extent of liver damage.
Some of the common treatments include:
- Lifestyle modifications like quitting alcohol, and weight management, as applicable.
- Medications and surgery, depending upon the stage and extent of liver damage. Treatment is aimed at controlling and preventing further damage (such as scarring) to the liver and managing symptoms and complications. When the complications cannot be controlled by treatment or surgery, liver transplantation becomes necessary.
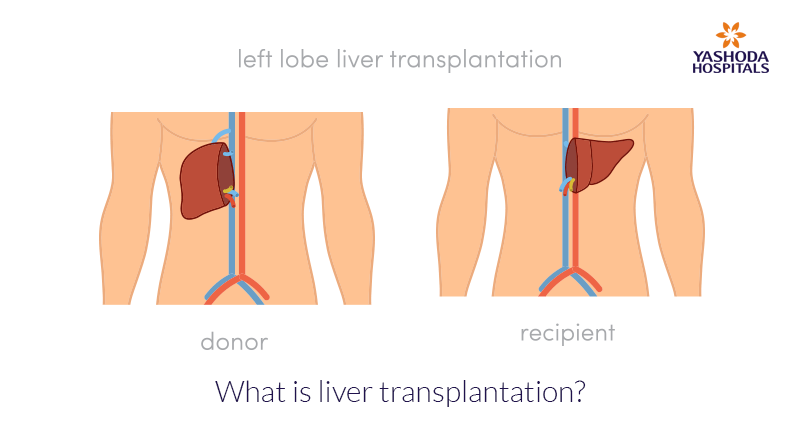
- Liver transplants: In patients with liver diseases especially, severe cirrhosis, end-stage liver disease and liver failure, a liver transplant may be needed. In liver transplant surgery, the patient’s diseased liver is replaced with either the whole or a part of a healthy liver from a donor. Liver transplant is an advanced surgery, performed by highly skilled liver transplant surgeons and a team of hepatologists. Some factors that affect the decision to do a transplant include:
- – Medical fitness: Since it is a major surgical operation, the patient should be medically fit to survive not only the operation, but also the potential post-operative complications
- – Adherence to treatments: Since, patients with liver transplant require long term medications. The patient should be able to adhere to the medication advice. Patient should be able to undertake frequent follow up visits and laboratory tests
- – Quit alcohol consumption: Patient should be motivated to not engage in harmful activities like drinking alcohol.
How can liver diseases be prevented?
Liver disorders may be prevented with a few lifestyle changes and precautions.
- Avoid heavy alcohol intake
- Avoid indulging in risky practices like intravenous drug abuse, unprotected sex etc.
- In case of accidental exposure to body fluids of a Hepatitis infected person, talk to your doctor or a gastroenterologist about getting vaccinated for Hepatitis B.
- Use the medications wisely, whether prescribed by your doctor or bought over-the-counter.
- Adopt safe practices whileusing sprays like insecticides, fungicides, toxic chemicals, paints etc.
- Maintain a healthy body weight
To know more about liver diseases/disorders and their treatment, you can request a callback and our liver specialists will call you and answer all your queries.
References:
- https://medlineplus.gov/liverdiseases.html
- https://www.mayoclinic.org/diseases-conditions/liver-problems/diagnosis-treatment/drc-20374507
- http://www.uptodate.com/contents/approach-to-the-patient-with-abnormal-liver-biochemical-and-function-tests
- The American Association for the Study of Liver Diseases, www.aasld.org
- The American Liver Foundation, www.liverfoundation.org