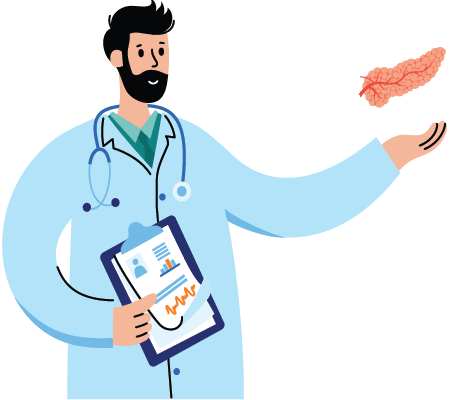
What is Pancreas Transplantation?
Pancreatic transplantation is a major surgical procedure in which a healthy pancreas, usually from a brain-dead donor, is implanted into a patient whose pancreas fails to produce insulin. This is usually a type I diabetic patient (as well as some type 2 diabetics) whose pancreas fails to produce the required insulin. This is a specialized procedure and is performed by a pancreas transplant surgeon.
Once the pancreas is removed from the donor, it is kept viable by cooling it and preserving it in an ice-cold preservative solution. It can be preserved only for a few hours after it is removed from the donor. In addition, the donor’s blood type must be compatible with the patient receiving the organ so that the body has a better chance of accepting the organ.
Who Requires a Pancreas Transplant?
For people with insulin-dependent diabetes who develop renal failure and are in need of kidney transplantation, transplantation of both pancreas and kidney is a viable option for better life and longevity. Some with insulin-dependent diabetes but with preserved kidney function can have other life-threatening complications and a poor quality of life. For them, pancreas transplantation alone is a reasonable option.
We accept physician referrals
and self-referrals.
What are the types of pancreatic transplants?
There are three types of pancreatic transplant options:
- Simultaneous Pancreas Kidney (SPK) Transplant:For insulin-dependent diabetes patients with kidney failure, kidney and pancreas transplantation can be done at the same time. Often, the pancreas and kidney will come from the same donor and be transplanted at the same time.
- Pancreas after Kidney (PAK) Transplant: In this case, kidney transplantation is done first, either from a living donor or a deceased (cadaver) donor. Pancreas transplantation is done after some time in a kidney recipient with a functioning kidney graft.
- Pancreas Transplant Alone (PTA): Pancreas transplants that do not require kidney transplants are for those who have severe, difficult-to-control (brittle) type I diabetes with life-threatening complications such as ketoacidosis, severe low blood sugar episodes (hypoglycemia and hypoglycemic unawareness) or other secondary complications with preserved kidney function. This procedure is also done in patients who undergo a total pancreatectomy.
What are the advantages of pancreatic transplants?
- With a functioning pancreas graft, you no longer require insulin injections. It will prevent complications such as ketoacidosis, dangerously low blood sugar levels, and low blood sugar (hypoglycemia) unawareness, thereby significantly improving quality of life.
- A functioning pancreas graft will protect the transplanted kidney from nephropathy and may increase the patient’s longevity. It will improve or stabilize other diabetic complications such as retinopathy (damage to the eye), neuropathy (damage to the nervous system), gastroparesis, and cardiovascular disease.
What are the risks of pancreatic transplants?
Some of the possible risks and complications that may result from a pancreas transplant are:
- It is a major surgical procedure and complications such as bleeding, blood clots, and infection can happen.
- Your body may reject the new organ as a foreign object and render it useless. You will have to take immunosuppressive drugs for the rest of your life to help prevent your body from rejecting the new organ. These drugs can lower your immune system and can have other side effects as well. However, if you are also having a renal transplant, you will be taking immunosuppressive medications anyhow.
Achievements
Dr. Srinivas Chava, Sr. Consultant – Liver Transplantation & Hepato Pancreato Biliary (HPB) Surgery, Yashoda Hospitals performed the first successful pancreas transplant (simultaneous pancreas and kidney transplant) in the states of Telangana and Andhra Pradesh on 17th October, 2014.