Precision Oncology: The New Frontier in Cancer Care
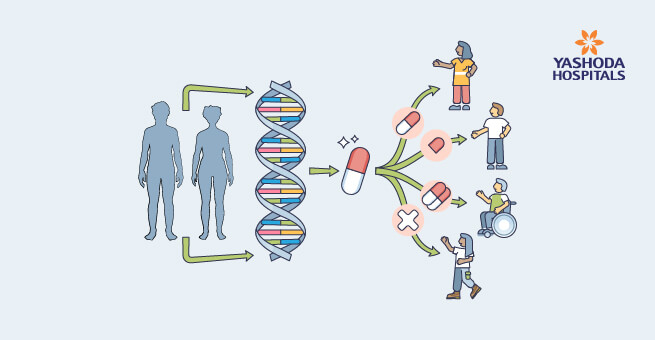
In our fight against cancer, envision a treatment tailored specifically for you—an approach uniquely designed not just for the type of cancer you have but precisely crafted to match the DNA and traits of your tumor. This is the groundbreaking reality of Precision Oncology, a pioneering approach reshaping how we combat cancer.
Unlike traditional methods, precision oncology isn’t a one-size-fits-all approach. It revolves around understanding the unique genetic makeup of each person’s tumour and utilizing that information to tailor treatments that are most effective. It’s about decoding the blueprint of cancer, unveiling its secrets at the molecular level, and using this knowledge to redefine the way we combat this complex disease.
But why is this considered the new frontier in cancer care? Because it marks a shift from the broad strokes of traditional treatments to a more targeted and individualised approach. It’s a game-changer, offering hope for better outcomes, fewer side effects, and a path towards truly personalized care for each and every cancer patient. Join us on this journey as we unravel the significance and potential of precision oncology.
The Heterogeneity of Cancer
Cancer, in its complexity, exhibits a spectrum of variations. Even within the same type of cancer, tumors can be remarkably different. For example, two people with the same type of cancer can have tumours that behave differently, respond differently to treatments, and have different genetic make-ups. This phenomenon, known as cancer heterogeneity, makes treating cancer uniformly challenging.
Traditional treatments like surgery, chemotherapy, and radiation, while potent, often fall short in addressing these unique differences in tumors. They may come with side effects and limitations, underlining the necessity for a more personalized approach.
To put it simply, if each tumor is like a fingerprint, precision oncology aims to read and understand these distinct patterns. By acknowledging the diversity among cancers, precision oncology seeks to tailor treatments to match the specific characteristics of each individual’s tumor.
Genomic Profiling: Decoding the Blueprint
At the heart of precision oncology lies genomic profiling, a transformative approach that decodes the unique genetic makeup of tumours. It relies on cutting-edge technologies like Next-generation sequencing (NGS), which serves as a powerful tool that enables a comprehensive analysis, identifying specific genetic mutations, alterations, and variations crucial for tailoring personalized treatment strategies with unprecedented precision and speed.
Identifying these genetic variations isn’t just about gathering information; it’s about making informed decisions. By understanding these genetic intricacies, doctors can tailor treatments more precisely, aiming directly at what makes each cancer grow and develop. This targeted approach can potentially lead to more effective and personalized cancer treatments, offering better outcomes for patients.
Targeted Therapy for Cancer: The Foundation of Precision Medicine
Unlike traditional chemotherapy, which can affect both healthy and cancerous cells, targeted therapies specifically target cancer cells. They directly interfere with the molecules or pathways that cancer cells depend on to grow and survive. By targeting these specific vulnerabilities, targeted therapies can stop or slow down the growth of cancer cells without causing as much harm to healthy cells.
The effectiveness of targeted therapies lies in their precision. They often come with fewer side effects compared to traditional treatments because they focus solely on the cancer cells. It not only fights the cancer but also minimises the impact on the body, allowing patients to maintain a better quality of life during treatment.
For patients, targeted therapies can mean more effective treatments with fewer side effects. It’s a game-changer, offering hope and better outcomes by tailoring treatments to fit the unique characteristics of each person’s cancer. While not every cancer type has targeted therapies available, ongoing research is expanding these options, bringing new hope to the fight against cancer.
Biomarkers: Guiding Treatment Decisions
Biomarkers play a crucial role in predicting how a person’s cancer might respond to different treatments. These could be certain proteins, genetic mutations, or other molecules that help understand how a particular cancer might behave. By analyzing these markers, doctors can personalize treatment plans, selecting therapies that are more likely to be effective for that individual. It’s like having a personalized roadmap, guiding doctors towards the most suitable treatment options.
One notable example of biomarkers in action is the use of HER2 in breast cancer. HER2 is a protein found on the surface of some breast cancer cells. Testing for HER2 status helps doctors identify patients who might benefit from targeted therapies specifically designed to attack cells with this marker, leading to more effective treatment. Another example involves genetic mutations like BRAF in melanoma. Blood tests for cancer markers aid in identifying this mutation, allowing doctors to choose treatments that specifically target cancer cells carrying this genetic abnormality, increasing the likelihood of a successful outcome.
Understanding and utilizing cancer biomarkers in precision oncology isn’t just about finding clues; it’s about harnessing this information to tailor treatments that are more effective and less invasive. It is a step towards personalized care, in which each patient’s unique cancer characteristics guide treatment decisions, providing hope for a better prognosis.
Immunotherapy and Precision Oncology
Immunotherapy for cancer boosts the immune system, empowering it to recognize and attack cancer cells. When immunotherapy and precision oncology are combined, they create a dynamic synergistic effect. Precision medicine helps identify specific characteristics within a tumor, revealing vulnerabilities that can be targeted by immunotherapy. This approach improves the effectiveness of the immune system’s ability to target and destroy cancer cells.
This combination offers promising results, leading to longer remission periods, fewer side effects compared to traditional treatments, and even complete remission in certain cases. It’s a beacon of hope in the fight against cancer, showcasing how these innovative approaches working together can make a significant difference in patients’ lives.
Challenges and Future Perspectives for Precision Oncology

One big challenge is accessibility—not everyone has equal access to advanced genetic testing or targeted therapies. Plus, interpreting complex genetic information can be tricky, requiring specialized expertise. Another hurdle is the tumor’s ability to evolve over time, making it tough to keep treatments effective in the long run.
To overcome accessibility challenges, efforts are underway to make molecular testing for cancer more widely available and affordable. Training healthcare providers in interpreting genetic data and collaborating across specialties can bridge the expertise gap. Also, ongoing research focuses on understanding how tumors change, aiming to develop treatments that adapt to these changes.
The future of precision oncology is brimming with possibilities. Researchers are exploring innovative technologies that could lead to earlier detection of cancer, more tailored treatments, and better outcomes for patients. Furthermore, advances in artificial intelligence are assisting in genetic profiling and the analysis of massive amounts of genetic data, allowing doctors to make more precise treatment decisions.
Precision oncology’s evolving landscape is steering us towards a future where cancer might be treated more effectively and with fewer side effects, offering hope for a brighter tomorrow in the fight against this complex disease.
References:
- Precision Oncology https://www.nih.gov/about-nih/what-we-do/nih-turning-discovery-into-health/precision-oncology
- How Precision Oncology Helps Cancer Patients https://www.ctoam.com/precision-oncology/
- Heterogeneity and Cancer https://www.cancernetwork.com/view/heterogeneity-and-cancer
- Cancer heterogeneity: implications for targeted therapeutics https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3593543
- The Use of Targeted Therapies for Precision Medicine in Oncology https://academic.oup.com/clinchem/article/62/12/1556/5612042
- Targeted Therapy to Treat Cancer https://www.cancer.gov/about-cancer/treatment/types/targeted-therapies
- Biomarkers in the Era of Precision Oncology https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10046681/
- Biomarkers in Precision Cancer Immunotherapy: Promise and Challenges https://ascopubs.org/doi/10.1200/EDBK_280571
- The Role of Next-Generation Sequencing in Precision Medicine: A Review of Outcomes in Oncology https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6164147/
About Author –